To account for the diverse lived experiences and exposures of various populations, clinical research should be appropriately inclusive of racial and ethnic minority groups, as well as other populations experiencing health disparities, including sexual and gender minority or socioeconomically disadvantaged populations.
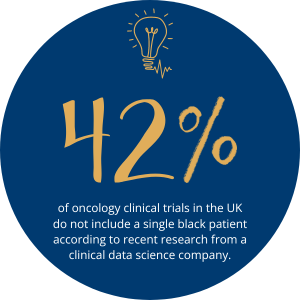
Forty-two percent of oncology clinical trials in the UK do not include a single black patient according to recent research from a clinical data science company. Analysis of 32,000 individuals who participated in new drug trials in the US in 2020 showed that only 8% were Black, 6% Asian, and 11% Hispanic. Clinical trials play a crucial role in the development of new medical treatments and therapies. Truly representative clinical trials will have benefits across the scope of clinical research, informing future strategies that will lead to more efficient, cost-effective, and equitable clinical trials. Increasing the participation of underrepresented groups in research can bring diverse lived experience, including sexual or gender minority or socioeconomically disadvantaged populations. The impact of limited diversity in clinical trials can have significant implications for the effectiveness and safety of new treatments, as different patient populations may respond differently to interventions. Ultimately, we must, as an industry, work to limit disparities in healthcare outcomes and the effectiveness of new therapies for the entire patient population.
Cpl Life Sciences took the opportunity to speak to multiple contacts within the field of clinical research patient engagement teams. While the majority of life sciences industry have processes in place to achieve diversity within trials, many professionals we spoke to indicated this was, disappointingly, often a “tick box” exercise. One of the greatest criticisms made by several of our commentators from industry and also patient advocate groups was the lack of follow-up with participating patients post-trial. This was seen as having a significant negative impact for both the patient and industry.
What contributes to underrepresentation in clinical research?
There are several factors that contribute to the underrepresentation of certain patient groups in clinical trials. Firstly, a lack of awareness and education can be a difficult area to confront. Many patients from underrepresented groups may not be aware of clinical trial opportunities or may have misconceptions about research studies. We saw this play out during the Covid pandemic with many ethnic or economically disadvantaged communities having a deep-rooted fear or scepticism around clinical trials and newly launched vaccines. This can often be based on the real lived experiences of families and the now well-known events such as the Tuskegee Syphilis study that crossed abhorrent ethical and economically disadvantaged population lines. A key challenge is continuing to reiterate that patient safety always comes first and the immense benefits of accessing ground-breaking medicines and enhanced care that is received in a clinical trial environment can be a substantial benefit.
How are underrepresented groups in clinical trials identified?
Some of the current strategies for identifying underrepresented patient groups are based on better community engagement. Getting back to building trust and relationships with communities through opening clinics in deprived areas, having easy-to-digest and understandable information advertised in GP surgeries and within patient advocacy groups, and for people to attend outreach programs, community events, and partnerships with community organisations can help increase awareness, trust, and participation in clinical trials. Ensuring all potential stakeholders are approached and engaged with from caregivers, family members, friends, clinical providers and administrators, community advocates, peers, religious leaders, and political figures.
Developing relationships with caregivers and family members is instrumental to recruitment and retention of underrepresented groups. For example, not talking to caregivers is a huge misstep. If you have populations that are vulnerable enough to have caregivers, they need to be engaged with as part of the trial. Community advisory boards and other strategies for eliciting community expertise can be a crucial element of protocol development and study execution. Conceptualising study participants as partners in research was an important component that required openness by the study teams to learn from the participants’ experiences and further endorse feedback Cpl Life Sciences gained from professionals within clinical research that following up patient participants in trials from underrepresented groups is critical for increasing adoption.
Finding underrepresented patient groups in clinical trials is essential for ensuring the generalisability and effectiveness of research findings. By implementing strategies to improve diversity and inclusion in clinical trials, researchers can better understand how treatments work across different patient populations and ultimately improve healthcare outcomes for all. It is crucial for the research community to prioritise diversity and equity in clinical trials to address disparities in healthcare and advance medical science.
Conclusion
In conclusion, it is apparent that the clinical development industry has a diversity problem. With constant challenges in recruitment and participation, certain groups are consistently underrepresented in clinical trials around the world. But these groups still fall ill, and they still need access to the latest therapies that are safe, efficacious, and accessible. We also know that due to genetic, social, and economic factors, certain patient demographics may be disproportionately affected by some health conditions or more prone to adverse reactions. Partnering with LGBTQA+ organisations and advocacy groups can help reach potential study participants who are interested in participating in clinical research. These organisations can also provide valuable guidance and support throughout the study.
Yet, due to a variety of factors including recruitment bias, the location of recruiting sites, and historical issues of mistrust, clinical trial participants are not always representative of the patient population. This means the industry is unable to develop effective therapies that benefit the entire population receiving drugs. We are now seeing some parts of the industry really stepping up to address diversity in clinical trials. The European Medicines Agency (EMA) updated its Clinical Trials Regulation to ensure sponsors justify any non-representative procedures followed by the US Food and Drug Administration (FDA), which issued new guidance on meaningful representation of racial and ethnic groups. To ensure these measures have the desired impact on trial participation, a patient-centric approach is needed. By harnessing the advanced technological capabilities now available, greater insights can be taken from data. We need to not see underrepresented groups as a “tick box” exercise, but as crucial to better outcomes for every community.
